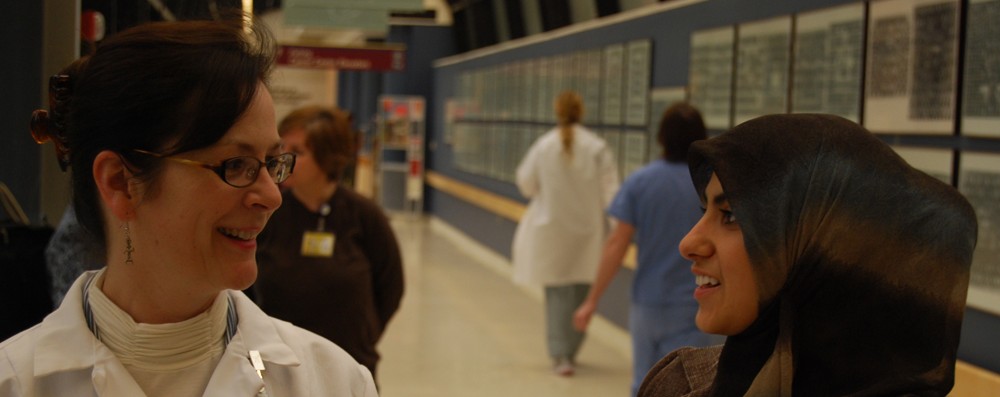
Presented December 19, 2014 by Linda Golley (Interpreter Services Manager, University of Washington Medical Center)
Medical interpreters, as any other health care worker, must be aware of what infection control means and know the measures that should be taken to prevent infection to and from a hospital setting as well as where to go to familiarize with health safety standards. INFECTION CONTROL is known as those measures taken to minimize the risk of becoming vectors of diseases to patients, family members, themselves, and any person the interpreter comes in contact with.
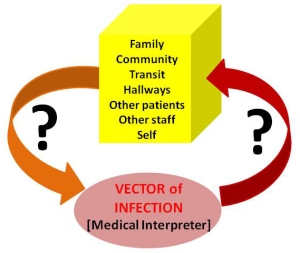
VECTORS OF INFECTION (carriers that transfer an infective agent from one host to another) can potentially be dangerous when vectors are not aware of the disease or infection they might be carrying. This could be due to the fact that they are merely mechanical carriers (they carry the infectious agent in their clothes, etc.), or when being biological carriers (they carry the infectious agent within their bodies), which in those cases is strongly related to the INCUBATION PERIOD (the symptoms of the disease are not yet manifested in them). Therefore, to prevent becoming a RESERVOIR OF INFECTION is recommended to get vaccinated when vaccines are available, and pay attention to each VACCINE EFFECTIVENESS TIME-LAPSE (vaccines are not immediately effective upon reception). The recommended vaccines for any healthcare worker are: MMR (Measles, Mumps, and Rubella); Chicken pox (Varicella); TDAP (Tetanus, Diphtheria, and Pertussis); Flu, annual; Hepatitis B; and TB (Tuberculosis) monitoring exposure, annual.
There are two types of Health Associated Infections (HAI), which sometimes are considered almost synonymous: Iatrogenic infections (originated during treatment) and Nosocomial infections (contracted in the hospital). In the USA, 2 million patients yearly get hospital related infections, with approximately 90,000 dying from them; and with most of those infections being transmitted on the hands of health care personnel. As might be expected, the most vulnerable populations to those infections are found within those very sick patients admitted in NICUs and ICUs, within those patients with depressed or suppressed immunologic systems (cancer patients, transplant patients, HIV/AIDS patients, and any other immune-suppressed – i.e., on steroids), or non-vaccinated patients.
In any situation, though, the best precaution is to assume that every patient/health worker is infected with a life-threatening blood-borne disease and with droplet-borne disease, and to act accordingly. Therefore, a self-conscious interpreter should always refuse assignments if he/she feels ill or experiences any disease symptoms.
Very important MEASURES/safety points to consider while on an assignment are:
- Take STANDARD PRECAUTIONS as peremptory with all patients.
- HAND HYGIENE, through; specific instructions are available at cdc.gov/handhygiene/
- ALWAYS FOLLOW POSTED signs as PRECAUTIONS outside the patients’ room; use always personal protective equipment (PPE) when prompted and/or advised to. And when remove PPE, leave it in the patient’s room; DO NOT take it into hallways.
- Use BARRIERS: physical – Positioning!!!
- DO NOT take food or drinks where patients are.
- AVOID SHAKING HANDS; you can always politely refuse by saying things in the style of: “You don’t want to shake hands with me; you don’t know where my hands have been!”.
TRANSMISSION-BASED PRECAUTIONS are especial extended precautions taken on top of standard precautions, not instead of. They are specific for every particular infectious organism.
Keep in mind that at ANYTIME the best measures to protect your patients are always to:
- Take nothing to their environments (room, etc.).
- Remove outer street clothing.
- Gel in and gel out (soap and water, if used continuously it dries up the skin and may cause skin cracks); to prevent that, it is advised to use gel provided by the facilities instead of interpreter’s own (composition is known, precludes handling personal stuff, and limits the number of surfaces touched before gelling).
- Touch nothing.
INDUSTRIAL SAFETY deals with vulnerability AND responsibility. It refers to all those actions taken by health care workers, medical interpreters among them, in all those areas within a health care setting where their own safety, due to vulnerability, might be compromised during the exercise of their profession: infection control, radiation safety, mechanical safety, chemical safety (spills), patient’s fall, cold/heat weight (tolerance), physical danger (behavior), safety in a disaster while on the job, mental health (vulnerability in a locked Psychiatric Unit). Therefore, it is strongly recommended at anytime for the interpreter to increase self-protection to minimize vulnerability. The interpreter should always be vigilant and take the appropriate responsibilities by BEING PROACTIVE:
- Dress properly for each given situation
- Follow Department of Health (DOH) rules
- Be alert to special precautions
- Be alert regarding to protective equipment
- Pay proper attention to standard precautions
It goes without saying that in cases with patients in psychiatric units or in prisoner environments the interpreter should never be alone with the patient, both for general safety and to prevent any putative interference from the interpreter into the therapy.
*****
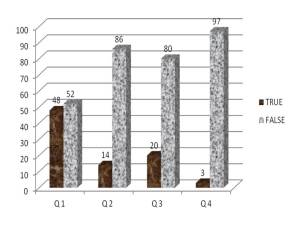
During the presentation the presenter posed four true or false questions to the audience:
- Is important for the interpreter to know what are the patients’ infections/diseases so interpreters can refuse an assignment?
- Medical interpreters are not dangerous to patients if they are careful to not shake hands with the patient.
- Medical interpreters are not dangerous to patients if they wear a surgical mask when they go to appointments while having a cough.
- Medical interpreters are not dangerous to patients if they put on a gown and a hair cover no matter what precautions are posted.
And these are the responses, in percentage, elicited by over 150 participants (being 66-74 % of them, Certified Interpreters):
The most controversial one among the four questions was doubtless the first one. I think that is very important for the interpreter to know the patient’s disease, and especially if it is infectious, but as the presenter pointed out, not to withdraw from the appointment, an action that should be prevented by the interpreters’ code of ethics, but to minimize the role of the interpreter as a vector of infection into and from the patient’s environment.
Resources:
- CCHI, Certification Commission for Healthcare Interpreters; http://www.cchicertification.org/
- CCHI Webinars: http://www.cchicertification.org/cchi-webinars/cchi-webinars
- Centers for Disease Control and Prevention (CDC); http://www.cdc.gov/
- S. Department of Health and Human Services (DOH); http://www.hhs.gov/
- Accreditations (Body Regulations for Hospitals and Clinics); Rules of each Specific Health organization.