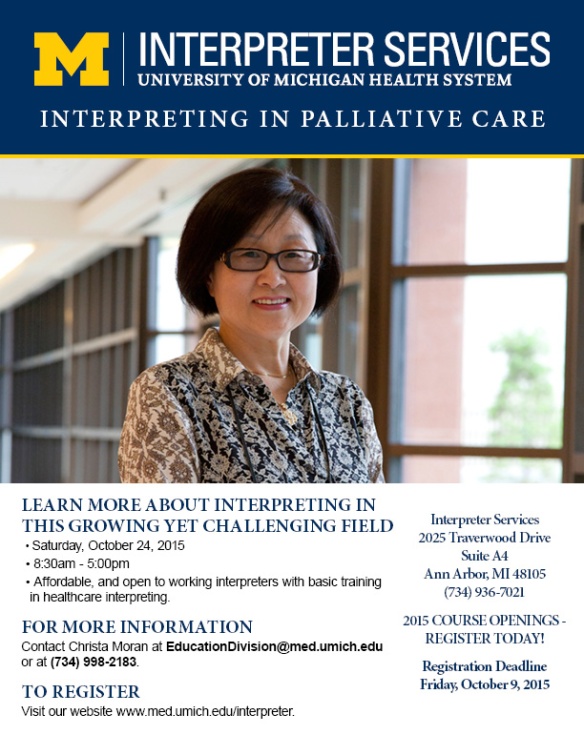
Interpreting in Palliative Care – 2015
Image
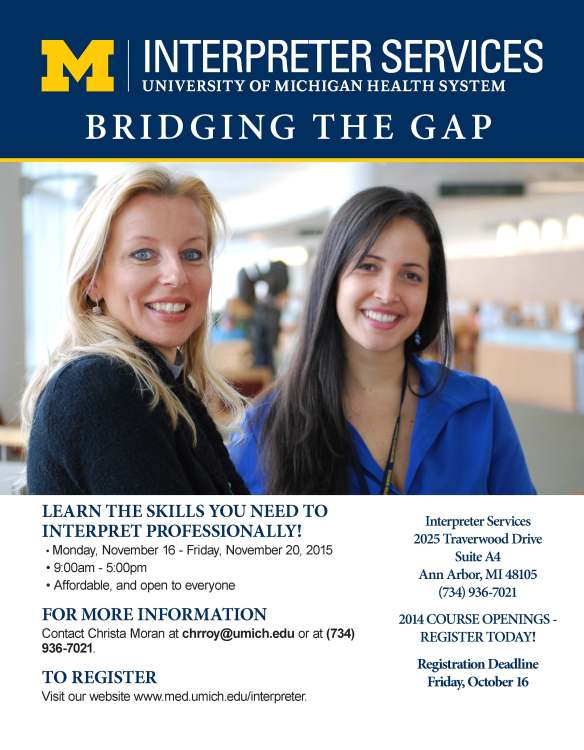
Register today for Foundations of Medical Interpreting – Fall 2015
Image
Medical Terminology & Body Systems – Fall 2015
Image
Mind Mapping: A Technique towards Improving Knowledge of Concept Relationships
In health care, medical providers usually specialize in certain areas of expertise where they are at ease regarding anatomical systems, putative diagnostics, and technical vocabulary. Healthcare interpreters, on the contrary, are highly generalist on what comes to specialized terminology, and on top of that they have to be exceedingly fluent in more than one language. As anybody who works in this field might be aware of, in getting into the profession of medical/healthcare interpretation, interpreters walk into a complex path composed not of well signaled highways but of intricate networks with unending multiple sidetracked looping ramifications.
Besides being familiar with the patients’ background culture (especially in dealing with languages such as Arabic, French, and Spanish, due to the high cultural diversity of their speakers) it is also expected that while on duty, for the healthcare interpreter to be well versed on the culture of medicine at large (diseases, diagnostic tools, procedures, techniques, equipment, protocols, medications); something that implies the need for continuous learning mainly by new knowledge acquisition through reading, and by attending specialized courses and seminars.
It was along those lines, and in order to help fellow interpreters get acquainted with useful techniques towards this goal that last winter, the CCHI Managing Director, Natalya Mytareva, presented within the CCHI’s online webinar series: Medical Terminology for Healthcare Interpreters: Disease, Disorders & Treatments of the Gallbladder. In there, using the gallbladder purposely as a mere example, she discussed some of the most up to date and innovative techniques developed with the background idea to help with vocabulary acquisition and terminology relationships.
Among those, mind mapping, although an ancient one, it has been proved a very useful technique in helping to relate ideas. Mind mapping mimics our brain’s ideas association patterns, and allow them to be portrayed as a diagram that uses a non-lineal graphical layout to construct intuitive frameworks around a central concept or subject.
Although a mind map may easily be drawn using pen and paper, software has been developed to such a goal and therefore, medical terminology relationships can effortlessly be established with the help of computerized frameworks, some of which can be accessed at:
- Free mind-mapping applications:
- Mindmup; for Chrome (desktop & Android)
- SimpleMind+; for Apple (iphone, ipad)
There are multiple possibilities for building a mind map around a particular concept, putative branches, ramifications, and sub-ramifications that can be presented as a whole or in sections, depending on what is aimed at to be highlighted at a given stage of a particular study.
As an example of how a mind map can be constructed to help increase knowledge of a particular organ or system, and to provide awareness of the multiple relations that can be derived from it you can see here, out of several possible ones, a mind map built around the core of the gallbladder.
In regards to suitable ideas, techniques, and exercises for gaining vocabulary and building up terminology to improve interpretation agility, always paying attention to words and intention, healthcare interpreters can:
- Online search in English and non-English language:
- Using search engines from countries of origin of non-English language
- Accessing websites from local reputable institutions
- Practice parallel text matching (find language equivalents and verify accuracy)
- Analyze components
- Check denotations (literal meanings)
- Check connotations (ideas of feeling, register, emotional charge)
- Look for word pictures
- Back-translation
And to help with those self-training endeavors serve this short list of available resources as starting point for anybody interested:
- https://translate.google.com/; for single words ONLY
- youtube.com; especially useful for watching functions & procedures
- Proz.com (The translation industry’s leading workplace)
- howjsay.com (A free online Talking English Pronunciation Dictionary)
- Asking people: ‘If I say this, what does it mean to you?’
- Language acquisition
- Practice consecutive and simultaneous interpretation
Now that you have the tools you just need to find yourself some time to put them to practice. Enjoy!